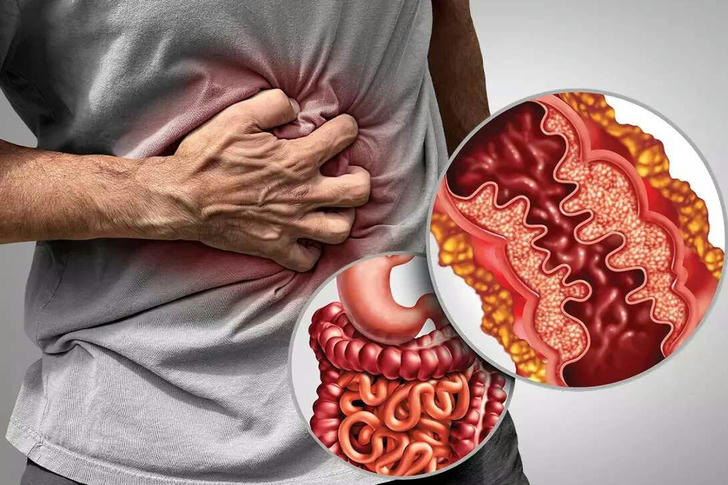
Always Tired, Bloated, and in Pain? It Might Be Crohn’s Disease
Stomach pain, diarrhea, weight loss... you think it's a gastrointestinal problem? It could be Crohn's disease!
It can occur at any age, with subtle but persistent symptoms that seriously affect the patient's quality of life. Millions of people around the world are suffering from it.
This guide will break down everything you need to know about Crohn’s disease — the symptoms and how to treat it.
🔍 What Exactly Is Crohn’s Disease?
Crohn’s disease is a type of Inflammatory Bowel Disease (IBD) that causes chronic inflammation in your gastrointestinal tract. While it can affect any part from your mouth to your anus, it most commonly targets the last part of the small intestine (ileum) and the first part of the colon.
🟥 Key Fact: Crohn's is a lifelong condition — there’s currently no cure.
Unlike occasional stomach pain or indigestion, Crohn’s is persistent, often painful, and can seriously interfere with daily life.
🚨 Common Symptoms (And Why You Shouldn’t Ignore Them)
Crohn’s symptoms can vary wildly from person to person. But here are the most common red flags:
- ⚠️ Persistent diarrhea (sometimes with blood)
- ⚠️ Cramping and abdominal pain
- ⚠️ Fatigue that won’t go away
- ⚠️ Unintended weight loss
- ⚠️ Fever
- ⚠️ Loss of appetite
- ⚠️ Anemia
🟥 If you’ve had 3 or more of these symptoms for weeks, you need to see a doctor.
🧬 Why Does Crohn’s Disease Happen?
Doctors are still not 100% sure what causes Crohn’s, but it’s likely due to a combination of:
| 🧪 Factor | 📝 Explanation |
|---|---|
| Genetics | People with close relatives with IBD are more likely to get it. |
| Immune system | The body attacks its own healthy gut tissue. |
| Environment | Smoking, pollution, and high-fat diets are linked. |
| Gut bacteria | Changes in gut microbiota may trigger abnormal inflammation. |
🟩 Interesting Note: Up to 20% of Crohn’s patients have a direct relative with IBD.
🔬 How Is It Diagnosed?
Diagnosis is often delayed, because symptoms mimic other gut problems like IBS or infections. Here's how doctors typically confirm Crohn's:
- Blood tests – To check for inflammation or anemia.
- Stool tests – To rule out infections.
- Colonoscopy – A camera checks your colon for inflammation.
- Biopsy – A tiny tissue sample confirms the diagnosis.
- CT/MRI scans – Show areas of inflammation, narrowing, or fistulas.
🟥 Don't self-diagnose Crohn's just because of stomach issues. Only tests can confirm it!
💊 Treatment Options: Medication/Surgery + Diet
There’s no cure (yet), but Crohn’s can be managed effectively with a combination of medications, diet, and sometimes surgery.
1. Medication
| 💊 Drug Type | 🔍 Purpose |
|---|---|
| Aminosalicylates (5-ASA) | Mild inflammation control |
| Corticosteroids | Quick relief during flare-ups |
| Immunomodulators | Suppress the immune system to prevent attacks |
| Biologics (e.g., Infliximab, Adalimumab) | Target specific proteins causing inflammation |
| Antibiotics | Treat infections or fistulas |
🟥 Biologics have revolutionized treatment but can be expensive and require close monitoring.
2. Diet and Nutrition
There’s no “one-size-fits-all” Crohn’s diet, but patients often find relief by avoiding:
- 🧀 Dairy
- 🌶️ Spicy foods
- 🍞 Gluten
- 🥬 High-fiber veggies during flare-ups
Low-residue diets can help reduce bowel movement frequency.
Pro Tip: Work with a registered dietitian familiar with IBD — your gut will thank you.
3. Surgery (When Medication Isn’t Enough)
Up to 70% of Crohn’s patients eventually need surgery due to:
- Narrowing (strictures)
- Abscesses or fistulas
- Severe inflammation
But surgery is not a cure — the disease often returns near the surgical site.
🟨 Example: A 2022 review found that 39% of patients who had surgery experienced disease recurrence within 5 years. [1]
🏥 Insurance & Coverage: What’s Actually Covered?
Treating Crohn’s isn’t cheap — but most insurance plans in the U.S. cover it.
- Private insurance usually includes doctor visits, colonoscopies, and meds like biologics (though 🟥 co-pays can be high and prior approval is often needed).
- Medicaid covers Crohn’s care in most states, but 🟥 step therapy rules may apply.
- Medicare helps with hospital care (Part A), outpatient visits (Part B), and meds (Part D).
- Drug makers often offer copay cards or patient assistance for expensive treatments like Humira or Stelara.
🟥 Don’t skip treatment due to cost — help is available.
👩⚕️ Living With Crohn’s: Daily Tips
Here are some daily-life survival tips from patients and experts:
- ⏰ Stick to a routine: Your gut likes predictability.
- 📝 Track your symptoms with a journal or app.
- 🚭 Quit smoking — it’s a known trigger for Crohn’s flares.
- 😌 Manage stress: Meditation, yoga, or therapy helps calm the gut-brain axis.
- 💧 Stay hydrated, especially if you have frequent diarrhea.
📊 Crohn’s vs. Ulcerative Colitis (Know the Difference)
| 🧾 Feature | Crohn’s Disease | Ulcerative Colitis |
|---|---|---|
| Area affected | Any part of GI tract | Colon only |
| Pattern | Patchy ("skip lesions") | Continuous inflammation |
| Depth | Full thickness of bowel wall | Only inner lining |
| Surgery outcome | Disease may return | Surgery may cure UC |
🟥 Don’t confuse Crohn’s with IBS or UC — they’re different beasts.
👶 Can I Still Have a Normal Life?
Yes! With proper management, many Crohn’s patients:
- Hold full-time jobs
- Have children
- Travel the world
- Run marathons
The key is early diagnosis, consistent treatment, and self-awareness.
🧠 Common Myths About Crohn’s
❌ It’s caused by stress or poor diet.
✅ False. While stress can worsen symptoms, it’s not the root cause.❌ It’s contagious.
✅ Nope. You can’t “catch” Crohn’s from someone.❌ Crohn’s is just a fancy name for diarrhea.
✅ Not even close. It’s a serious autoimmune condition that can lead to life-threatening complications.
🎯 Final Thoughts
Crohn’s disease is more than a stomach problem — it’s a life-altering autoimmune condition that affects everything from diet to mental health. But with the right care, you can live a full, vibrant life.
🟥 Don’t ignore the signs. Don’t settle for discomfort. Get diagnosed, get treated, and get your life back.
📚 References and Sources
- Hanauer SB. Inflammatory bowel disease: epidemiology, pathogenesis, and therapeutic opportunities. Inflamm Bowel Dis. 2006.
- NIH – National Institute of Diabetes and Digestive and Kidney Diseases
- Crohn's & Colitis Foundation
- Rubin DT, et al. ACG Clinical Guideline: Ulcerative Colitis in Adults. Am J Gastroenterol. 2019.
If you found this guide helpful, feel free to share it for someone who might be struggling silently. 💙
